ADHD: How many of us will end up being diagnosed?

 BBC
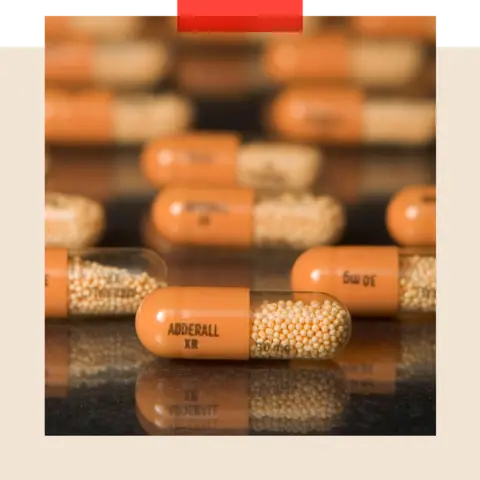
BBCThe number of people taking ADHD medication is at a record high – and the NHS is feeling the strain as it tries to diagnose and treat the condition.
Since 2015, the number of patients in England prescribed drugs to treat ADHD has nearly trebled, and BBC research suggests that it would take eight years to assess all the adults on waiting lists.
Last year, ADHD was the second-most viewed condition on the NHS website. Concern about this rising demand has prompted the NHS in England to set up a taskforce.
So what’s going on and where will it end? Is ADHD (attention deficit hyperactivity disorder) becoming more common? Are we just getting better at recognising it? Or is it being over-diagnosed?
It turns out it’s not just you and I who have been taken by surprise – so have the experts.
Dr Ulrich Müller-Sedgwick, the ADHD champion for the UK’s Royal College of Psychiatrists, says: “Nobody predicted that the demand would go up so massively over the last 15 years, and especially the last three years.” He’s been running adult ADHD clinics since 2007. At the time, he says, there were just a few of them.
ADHD is a fairly novel condition – it’s only 16 years since the National Institute for Health and Care Excellence (NICE) officially recognised it in adults. When considering whether it might keep increasing, Dr Müller-Sedgwick argues that there are two different concepts to consider: prevalence and incidence.
Prevalence is the percentage of people who have ADHD – Dr Müller-Sedgwick predicts that will stay pretty steady at 3 to 4% of adults in the UK.
Incidence is the number of new cases – people getting a diagnosis. That’s where we’re seeing an increase. He explains: “What has changed is the number of patients we are diagnosing. It’s almost like the more we diagnose, the more word spreads.”
 Getty Images
Getty ImagesProf Emily Simonoff echoes this. She is a child and adolescent psychiatrist at the King’s Maudsley Partnership for Children and Young People. She thinks about 5 to 7% of children have ADHD in the UK – and says: “It’s pretty similar across the world, that’s been consistent and it hasn’t actually risen.”
Prof Simonoff agrees that there’s been a “steep incline” in people coming forward for assessment since the pandemic – but says this comes after years of “long-term under-recognition”.
She points to statistics on ADHD drugs. She would expect about 3 to 4% of children in the UK to need ADHD medication, but in reality, only 1 to 2% are actually using it. She thinks this shows that we are still underestimating the scale of the issue.
Prof Simonoff explains: “I think that’s an important starting point for when we say, ‘My goodness, why are we seeing all these children now – are we over-identifying ADHD?’ We have under-diagnosed or under-recognised ADHD in the UK for many, many years.”
In other words, we can expect more people to be diagnosed with ADHD now because services are playing catch-up.
The ‘hump’
Thea Stein is chief executive of health think tank the Nuffield Trust. She’s got her own description for the recent increase in demand: “the Hump”. She says: “Diagnosis or desire to be diagnosed has risen because of knowledge and visibility – [it’s as] simple as that.”
According to Stein, the most immediate task is getting through the Hump, assessing the huge backlog of people on ADHD waiting lists. Then, in the longer-term, she thinks society will get better at spotting ADHD sooner in children. She hopes this will mean that they get better support from an early age, and take some of the pressure off adult services.
She says: “I have real optimism that we will come through this period of time to a much better place as a society. What I don’t have optimism about is that this is a quick fix.”
ADHD might be a new concept, but people struggling to concentrate is an old problem.
In 1798, Scottish doctor Sir Alexander Crichton wrote about a “disease of attention” with “an unnatural degree of mental restlessness.”
He explained: “When people are affected in this manner… they say they have the fidgets.”
ADHD goes beyond problems concentrating or being hyperactive, though. People with it can struggle regulating their emotions and impulses. It’s been linked to substance abuse and financial difficulties as well as higher rates of crime and even car crashes.
All the experts I speak to firmly agree on one point: it is much better for someone with ADHD to be diagnosed and treated as early as possible.
Dr Müller-Sedgwick says there’s a “risk of really bad outcomes”. But he lights up when he describes how diagnosis and treatment can transform lives.
He says: “I have seen so many patients getting better, getting back into work or back into education. I have seen parents who were going through family court proceedings who were able to be better parents.
“That’s why we work in this field, it’s a really rewarding part of mental health to work in.”
Breakthroughs in treatment
Currently, ADHD treatment revolves around medication and therapy, but there are other options on the horizon.
A patch worn by children with ADHD on their foreheads during sleep – connected to a device that sends stimulating pulses into the brain – is on sale in the United States. It’s not prescribed in the UK, but academics here and in the US are working on clinical trials looking into it.
Prof Katya Rubia is a professor of cognitive neuroscience at King’s College London – as she puts it, “My work over the last 30 years or so is basically imaging ADHD, understanding what is different in the brains [of people with ADHD].”
She explains that certain parts of ADHD brains, including the frontal lobe, are slightly smaller and also less active. Prof Rubia is trying to kickstart those areas of the brain, and is working on a study looking at the trigeminal nerve – it goes directly to the brain stem and can increase activity in the frontal lobe.
She says: “This is all very new. If we find an effect, we have a new treatment.” While that is yet to be proven, she does add: “If everything goes well, it could be on the market in two years.”
So, the hope is that, in the not-too-distant future, there will be more ways to treat ADHD without medication. In the meantime, though, the challenge is getting through that “hump” of people waiting to be assessed – with the belief that, over time, the increase in diagnoses should lessen.
See BBC Action Line for support on issues around ADHD
Top picture: Getty Images
BBC InDepth is the new home on the website and app for the best analysis and expertise from our top journalists. Under a distinctive new brand, we’ll bring you fresh perspectives that challenge assumptions, and deep reporting on the biggest issues to help you make sense of a complex world. And we’ll be showcasing thought-provoking content from across BBC Sounds and iPlayer too. We’re starting small but thinking big, and we want to know what you think – you can send us your feedback by clicking on the button below.










